Mastering the Rotablator: Essential Insights for Effective Atherectomy
Have you ever wondered why some angioplasty procedures don’t work on severely blocked arteries? That’s where the rotablator comes in. Treating heavily calcified coronary lesions is one of the toughest jobs in cardiology. These stubborn plaques can resist regular balloon angioplasty, making stent placement nearly impossible.
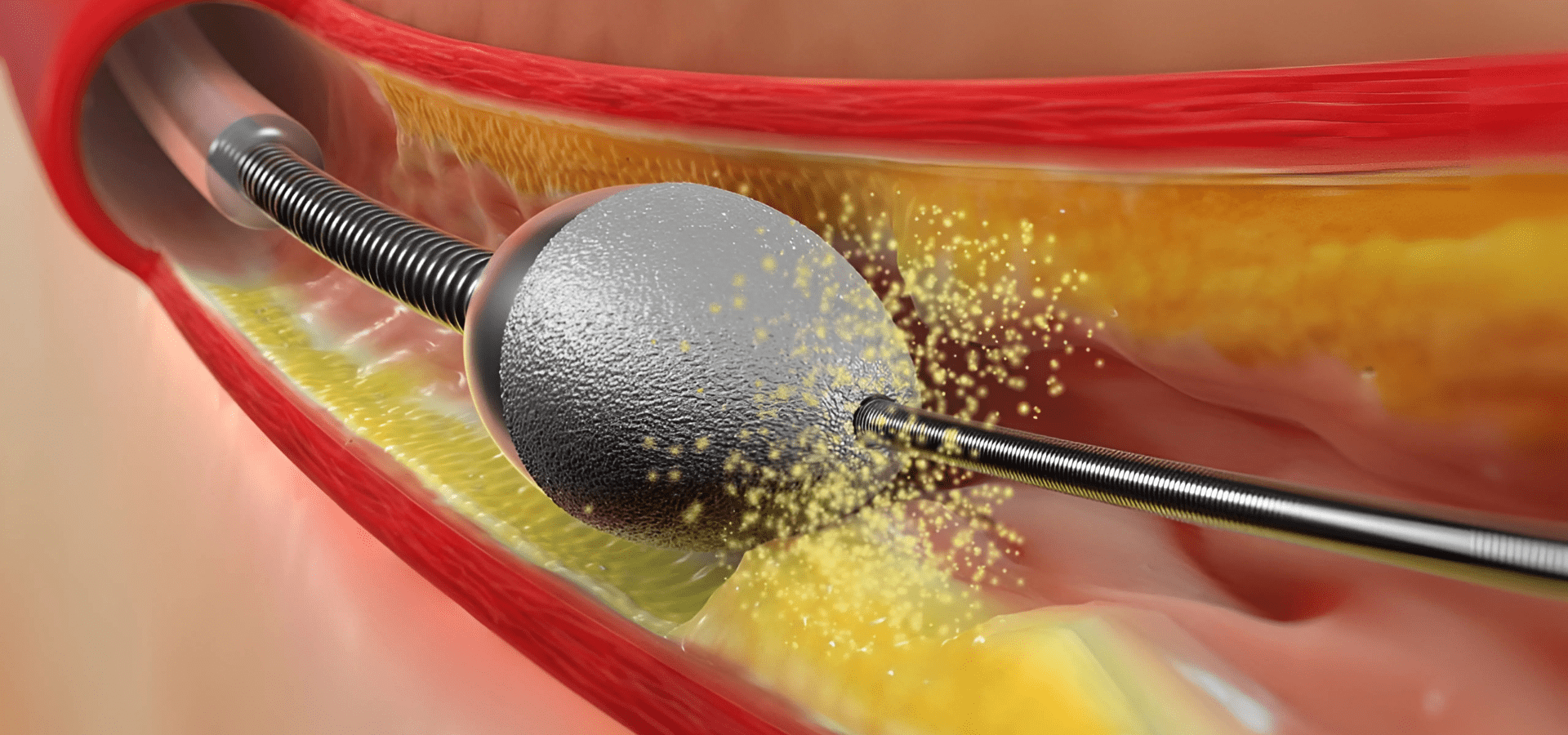
Rotational atherectomy, often called rotablation, is the tool specialists use when nothing else works. This technique drills through hardened plaque using a diamond-tipped burr, allowing better stent delivery and improved blood flow. Let’s decode how to master this tool and when to use it for the best outcomes in percutaneous coronary intervention (PCI).
What Is Rotational Atherectomy (RA) and Why Is It Needed?
Rotational atherectomy, also known as the rotablator procedure, is a technique to break down calcified plaque inside coronary arteries. These plaques are too hard for standard balloon angioplasty. The rotablator spins at high speed, grinding the plaque into tiny particles.
This clears the path for successful stent implantation. The need arises in cases with severe calcification where conventional methods fail. Using a rotablator in such situations increases the success rate of PCI and reduces complications. It’s now a go-to approach for complex coronary lesions and high-risk patients with chronic total occlusions.
What Makes Rotational Atherectomy Essential in Treating Calcified Coronary Lesions?
Rotablation is often the last resort before bypass surgery. When arteries are clogged with calcium, it’s like trying to inflate a balloon inside a rock. No expansion. No blood flow improvement. Stents can’t open well, and the result is poor.
In heavily calcified lesions, especially in the left anterior descending artery or circumflex artery, standard techniques just don’t cut it. Rotablation modifies these lesions. It makes the artery wall more flexible, enabling smoother stent delivery and proper expansion. Studies show higher procedural success rates and fewer major adverse cardiovascular events with RA.
In India, where lifestyle diseases lead to early-onset coronary artery disease, this method offers a lifeline. Patients with diabetes, previous stents, or those who have had prior bypass grafts often present with severely calcified coronary arteries. RA improves the clinical outcome in such high-risk cases. It also reduces the chances of vessel perforation or poor stent expansion. So, when you’re dealing with rigid calcium that resists even high-pressure balloon dilatation, rotablation angioplasty changes the game.
How Rotablation Works: Key Mechanism and Components
Rotablation uses a simple yet powerful principle: differential cutting. The rotablator burr, coated with microscopic diamonds, rotates at 140,000–200,000 rpm. It pulverizes calcified plaque into tiny particles smaller than red blood cells, which pass safely into the bloodstream.
Mechanism:
The rotating burr ablates calcified tissue but spares the soft arterial wall. That’s what makes this tool so precise. The operator uses a special console, compressed air source, and guiding catheter to control the burr’s movement. The process allows for lesion modification without damaging the healthy artery.
Key Components:
- Rotablator Burr: Comes in sizes 1.25 to 2.0 mm. Chosen based on lesion severity.
- Rotablator Console: Controls burr speed and rotation direction.
- Compressed Air Source: Powers the burr rotation.
- Guiding Catheter: Channels the burr and wires into the coronary artery.
- Advancer: Moves the burr forward in short, pecking strokes.
- RotaWire: A specialized, flexible wire that allows burr passage.
Additional Tools:
- Intravascular Ultrasound (IVUS): Helps visualize plaque and artery wall.
- Drug Eluting Stent (DES): Deployed after plaque debulking.
- Balloon Catheter: Used after RA for post-dilatation.
During the procedure, the interventional cardiologist ensures slow, controlled forward motion to avoid complications like vessel dissection or perforation. Saline flush, heparin, and vasodilators are also administered to minimize thrombus and vessel spasm.
Inside the ROTAPRO™ System: Equipment and Setup
ROTAPRO™ is the latest and most user-friendly version of the rotablator system. Designed for better ergonomics and efficiency, it simplifies the complex setup traditionally associated with rotational atherectomy.
Key Features:
- All-in-One Console: Combines compressed air, burr control, and foot pedal input.
- Simplified Tubing System: Quicker connections and fewer errors.
- Ergonomic Advancer: Easy one-handed operation.
- Visual Display: Real-time burr speed, pressure, and alerts.
Step-by-Step Setup:
Patient Preparation:
- Standard coronary angiography to locate the lesion.
- Choose the right guiding catheter and rota burr size.
- Intravascular ultrasound (if available) to assess plaque burden.
System Assembly:
- Attach the ROTAPRO console to a compressed air source.
- Connect the drive shaft, saline flush system, and foot pedal.
Wire Navigation:
- Insert RotaWire into the artery under fluoroscopy.
- Carefully cross the lesion using a microcatheter.
Burr Advancement:
- Mount burr over the RotaWire.
- Activate the console and start burr rotation.
Atherectomy:
- Use pecking motion.
- Watch for deceleration. Stop if it drops more than 5,000 rpm.
Post-RA Work:
- Withdraw burr carefully.
- Perform balloon angioplasty if required.
- Deploy a drug eluting stent.
ROTAPRO™ has made it easier even for less experienced centers to adopt rotablation safely. Its intelligent system minimizes user errors and helps reduce complications.
Step-by-Step: Performing RA in Practice
Mastering the rotablator requires more than knowing the equipment. It demands understanding patient risk, artery anatomy, and every nuance of coronary angiography. Clinical practice shows that a structured, step-wise approach ensures success, even in complex coronary artery disease.
1. Patient Selection and Pre-Procedure Planning
Identifying the right patient is critical. Look for signs of heavily calcified lesions during coronary angiography. This includes radio-opaque plaque, balloon failure, or non-dilatable areas. Patients with stable angina, chronic total occlusions, or those post-bypass surgery are common candidates. Consider risk factors like age, diabetes, previous stent implantation, and renal function. Use intravascular ultrasound (IVUS) or OCT imaging for accurate plaque burden assessment.
Ensure labs check creatine kinase and renal markers. A thorough briefing with the patient is essential. Explain the rotablator procedure, risks, and stent implantation steps. Pre-load medications such as aspirin, clopidogrel, and statins. If needed, use intra-aortic balloon pump support for high-risk cases. Proper planning improves outcomes and minimizes complications.
2. Guide Catheter and Wire Placement
Choose the guiding catheter carefully, good support is crucial. Extra backup (XB) or Amplatz Left (AL) catheters often work well. Engage the coronary ostium gently to avoid trauma. Insert the RotaWire under fluoroscopy, ensuring it crosses the calcified lesion smoothly. If it doesn’t, use a microcatheter to help. Position the wire tip in the distal vessel segment.
Avoid sharp bends or kinks. Proper wire placement improves burr control and reduces risk of perforation. Always double-check positioning before proceeding. Use small injections of contrast to confirm vessel anatomy. Remember, a stable guide and wire setup forms the backbone of a safe and successful rotablation angioplasty.
3. Burr Selection and Operation Technique
Choose the smallest effective burr size. Typically, 1.25 mm or 1.5 mm works for most lesions. Larger burrs increase the risk of complications. Before starting, flush the system with heparinized saline. Start burr rotation at 160,000–180,000 rpm. Use a pecking motion, short 15-second forward moves. Never push hard.
Let the burr do the work. Monitor rpm drop, stop if it drops more than 5,000 to avoid burr stall. Watch for excessive friction, which may damage the vessel wall. Maintain continuous flush with vasodilators to prevent spasm. Avoid burr passage through soft plaque or bifurcations. If resistance feels high, withdraw and reassess. Rotablator success depends on technique finesse, not aggression.
4. Adjunctive Balloon Angioplasty and Stent Placement
After rotablation, remove the burr and inspect for debris or kinks. Then perform low-pressure balloon dilatation to open the vessel further. Choose semi-compliant or non-compliant balloons, depending on lesion recoil. Balloon angioplasty improves lesion preparation before stent delivery. Next, choose the right drug eluting stent. Ensure full coverage of the treated vessel. Use intravascular ultrasound to confirm stent sizing and apposition.
Deploy the stent slowly and steadily. Then post-dilate using a high-pressure balloon to reduce residual stenosis. Full expansion is key. Under-expanded stents lead to restenosis and major adverse cardiovascular events. The final angiographic run should show good blood flow, minimal dissection, and no perforation.
5. Post-Procedure Monitoring and Follow-Up
Shift the patient to the ICU or monitored care. Watch for signs of vessel injury, ECG changes, chest pain, or hypotension. Monitor creatine kinase levels to rule out myocardial injury. Continue dual antiplatelet therapy for stent maintenance. Educate the patient about symptoms like recurrent angina. Schedule follow-up with coronary angiography if needed.
For complex cases, recommend cardiac surgeon consultation or additional imaging. Regular follow-up ensures sustained clinical outcomes. Encourage lifestyle changes, diet, exercise, and smoking cessation to prevent restenosis. In India, where compliance can be challenging, involving family in post-discharge care improves adherence. Rotablation isn’t the end; it’s the beginning of better-managed coronary artery disease.
Advanced RA Strategies for Complex Cases
Sometimes, calcified lesions are not straightforward. These are not your regular PCI cases. You may be dealing with long segment disease, bifurcation points, or even the left main stem. That’s when advanced techniques become critical. Rotablation, in these settings, must be adapted thoughtfully. Precision matters more than speed. Below are specific sub-strategies that experts follow when facing tougher scenarios.
1. Tackling Ostial and Left Main Lesions
Ostial and left main lesions carry higher risks. These are large-caliber arteries. Any misstep can affect a significant myocardial territory. Always use a larger guide catheter for better support. Choose the burr cautiously, often starting with 1.25 mm.
Ensure stable guiding catheter engagement. Avoid burr jumping by maintaining a slow, steady advancement. Use temporary pacing if the bradycardia risk is high. Balloon angioplasty post-RA should be gentle but effective. IVUS guidance is almost mandatory here. Stent expansion must be complete, as incomplete coverage can lead to severe restenosis or complications like stent thrombosis.
2. Dealing with Long and Tortuous Lesions
Long lesions often require more time and more planning. Do not attempt to cover everything with one burr pass. Divide the segment and address in stages. Use smaller burrs and increase size cautiously if required. Tortuous paths need guide support and wire positioning with extra care.
Avoid aggressive angulation, the vessel perforation risk is higher. Consider guide extension catheters for distal reach. Re-crossing long calcified segments with a balloon post-RA may still need careful coaxial alignment. Never rush this step. Patience pays off in these challenging cases.
Rotational Atherectomy Outcomes: What the Evidence Shows
Rotablation is no longer an experimental add-on. It’s proven. Decades of clinical follow-up, registry data, and randomized studies back it. What matters is how consistently RA improves results in complex lesions. Below are highlights of what the data tells us about procedural success, long-term effects, and comparisons to traditional methods.
Procedural Success Rates
- Rotablation shows an over 95% success rate in experienced hands.
- It drastically improves stent delivery and expansion in heavily calcified lesions.
- Higher rates of complete lesion modification allow for better drug-eluting stent implantation.
- Especially useful in complex coronary artery disease, like left main stem and chronic total occlusions.
- Reduces need for open heart surgery or bypass surgery.
- Rotablator stent procedures show improved blood flow with less residual stenosis.
Clinical Outcomes and Long-Term Benefits
- One-year clinical follow-ups show reduced major adverse cardiovascular events.
- DES implantation after RA leads to lower restenosis.
- Better quality of life reported in patients with severely calcified coronary lesions.
- Lower rates of re-hospitalisation for angina or myocardial infarction.
- RA also helps in managing high-risk patients who aren’t fit for surgery.
- Better outcomes reported in stable angina and multi-vessel disease cases.
Comparative Studies with Balloon Angioplasty and OA
- Traditional balloon angioplasty often fails in extremely calcified lesions.
- Orbital atherectomy (OA) offers an alternative, but may be less predictable in very hard lesions.
- Rotablation still holds the edge in procedural versatility and tool availability.
- RA has wider global usage, with more training and expertise available.
- Studies support the rotablator procedure over standalone balloon dilatation for complex calcified coronary lesions.
- IVUS and coronary angiography post-RA show better plaque modification than OA.
Complications and How to Minimize Them
No medical procedure is without risks. Rotablation, though effective, has its own set of complications. But here’s the good news, most of them are predictable and preventable with sound technique and careful monitoring. Understanding what could go wrong helps you avoid it altogether. Below are the most common issues and strategies experts use to reduce their impact.
1. Slow Flow and No-Reflow Phenomenon
Slow flow or no-reflow happens when micro-particles released during plaque modification clog the distal vessel. Blood flow drops suddenly. It’s dangerous. You’ll see ECG changes and chest pain. This issue usually occurs if the burr is advanced too aggressively or used for long durations. The fix? Short bursts—15 to 20 seconds max.
Always keep the burr moving gently. Never stall. Flush with vasodilators like verapamil or nitroglycerin. Use continuous heparinised saline to prevent debris buildup. Consider an intra-aortic balloon pump if the patient is unstable. Also, ensure proper hydration before the procedure. Watch contrast use. A clean technique with minimal contrast saves kidneys and prevents further complications. IVUS can help assess vessel diameter and reduce aggressive burr selection. Slow flow is preventable with the right habits.
2. Burr Entrapment or Stalling
This one’s a nightmare. Burr entrapment can stop your case cold. It happens when the burr gets stuck inside a calcified segment or bifurcation. Avoid by using the right size burr—never oversize. Start small, then upsize gradually if needed. Don’t push against resistance. Burr should glide, not grind. Use pecking motion, not continuous drive. If entrapment happens, reverse the drive with the console gently while maintaining wire tension. Sometimes you’ll need to pull the whole assembly out. If that fails, surgical help may be needed. Proper wire placement and angulation are critical. Always prepare a bailout strategy before you start complex cases. Having a standby cardiac surgeon or hybrid OR in tertiary centers is good practice.
3. Vessel Perforation and Dissection
Perforation is rare but serious. It can happen if you use a large burr or push too hard. Also, tortuous arteries and sharp angles increase the risk. Dissection often results from poor burr control or jerky movements. Avoid using the rotablator burr in vessels under 2.5 mm unless absolutely necessary. Confirm artery size using IVUS.
Use the smallest burr that still gives you plaque modification. Advance with slow pecking. Never rush. If perforation occurs, tamponade with balloon inflation and alert surgical backup. Covered stents may also be used in some cases. Always have emergency drugs and blood units ready. Monitor for pericardial effusion and tamponade. Fast action can save the patient. This is why experience matters. Senior operators know when to stop and reassess.
RA vs. Other Atherectomy Techniques: OA and ELCA
While RA is widely used in India and globally, it’s not the only method for lesion modification. Other atherectomy techniques include Orbital Atherectomy (OA) and Excimer Laser Coronary Atherectomy (ELCA). Each has its advantages and limitations depending on lesion type, operator experience, and availability. Here’s a quick comparison:
| Feature | Rotational Atherectomy (RA) | Orbital Atherectomy (OA) | Excimer Laser Coronary Atherectomy (ELCA) |
|---|---|---|---|
| Mechanism | Diamond-tipped burr rotation | Eccentric crown orbital motion | Pulsed ultraviolet laser energy |
| Best For | Severely calcified concentric lesions | Calcified lesions with tortuosity | In-stent restenosis, fibrotic lesions |
| Burr/Wire Type | RotaWire and burr (1.25–2.0 mm) | ViperWire and crown (1.25–2.0 mm) | Laser catheter (various sizes) |
| Speed | 140,000–200,000 rpm | 80,000–120,000 rpm | Pulsed bursts (non-mechanical) |
| Lesion Entry | Moderate learning curve | Slightly easier, gentle entry | Steep learning curve |
| Effectiveness in Severely Calcified | High | Moderate to high | Low to moderate |
| Device Availability in India | Widely available | Limited centers | Available in select tertiary centers |
| Operator Expertise Required | High | Moderate | Very high |
| Risk of Vessel Injury | Moderate | Low to moderate | Low |
| Additional Imaging Needed | IVUS recommended | IVUS helpful | OCT and IVUS needed |
| Cost | Moderate | High | High |
| Suitability for Complex Lesions | Excellent | Good | Limited |
RA stands out for its long-standing use, availability, and predictable outcomes, especially in severely calcified coronary lesions. OA is emerging, especially in U.S. and European practices. ELCA is reserved for select situations and not preferred for plaque debulking. In Indian clinical practice, rotablator systems remain the workhorse for treating complex coronary artery disease.
SRM Global Hospitals: Supporting RA Excellence
SRM Global Hospitals is not just another cardiac center. It is a referral hub for managing complex coronary lesions, especially severely calcified ones that need rotablation. With access to the latest ROTAPRO™ systems, IVUS imaging, and a dedicated team of interventional cardiologists, the hospital has positioned itself as a leader in precision-based coronary angioplasty.
Our cardiac team includes specialists trained in handling challenging cases, whether it’s rotablator stent implantation in high-risk patients or managing complications like vessel perforation and dissection. Each case is reviewed in detail, combining intravascular imaging with expert opinion for better clinical outcomes. We also work closely with cardiac surgeons when hybrid strategies are needed.
The catheterization labs are equipped with real-time monitoring and emergency backup, including intra-aortic balloon pumps and surgical support, ensuring patients receive safe, effective, and timely care.
If you or a loved one is struggling with complex coronary artery disease, don’t wait.
Book your appointment today with SRM Global Hospitals for the right advice, experienced hands, and world-class facilities that deliver the best results in rotablation angioplasty.
Conclusion
Rotational atherectomy with the rotablator is more than just a niche procedure, it’s a lifesaving option for patients with calcified coronary arteries who have no other option. When done right, it dramatically improves stent delivery, expansion, and long-term results. But it’s not just about having the right tool. It’s about knowing how and when to use it.
At the hands of an expert, with careful planning, modern equipment, and clinical experience, RA can transform outcomes for patients who were once inoperable. Choose the right center, the right team, and the right approach. Choose excellence.
FAQs
1. Is rotablation angioplasty safe for elderly patients?
Yes, especially when done in experienced centers. It helps avoid bypass surgery.
2. What’s the rotablation success rate in India?
Success rates exceed 90% when performed with proper technique and planning.
3. Does the rotablator damage the artery wall?
No. It selectively ablates calcified plaque, sparing soft tissue.
4. Can I get a drug eluting stent after RA?
Yes. In fact, it improves stent delivery and expansion significantly.
5. Is rotablation used for chronic total occlusions?
Yes, particularly when the lesion is severely calcified and cannot be crossed with balloons.






