Esophageal Varices: What Happens When Blood Flow Is Blocked
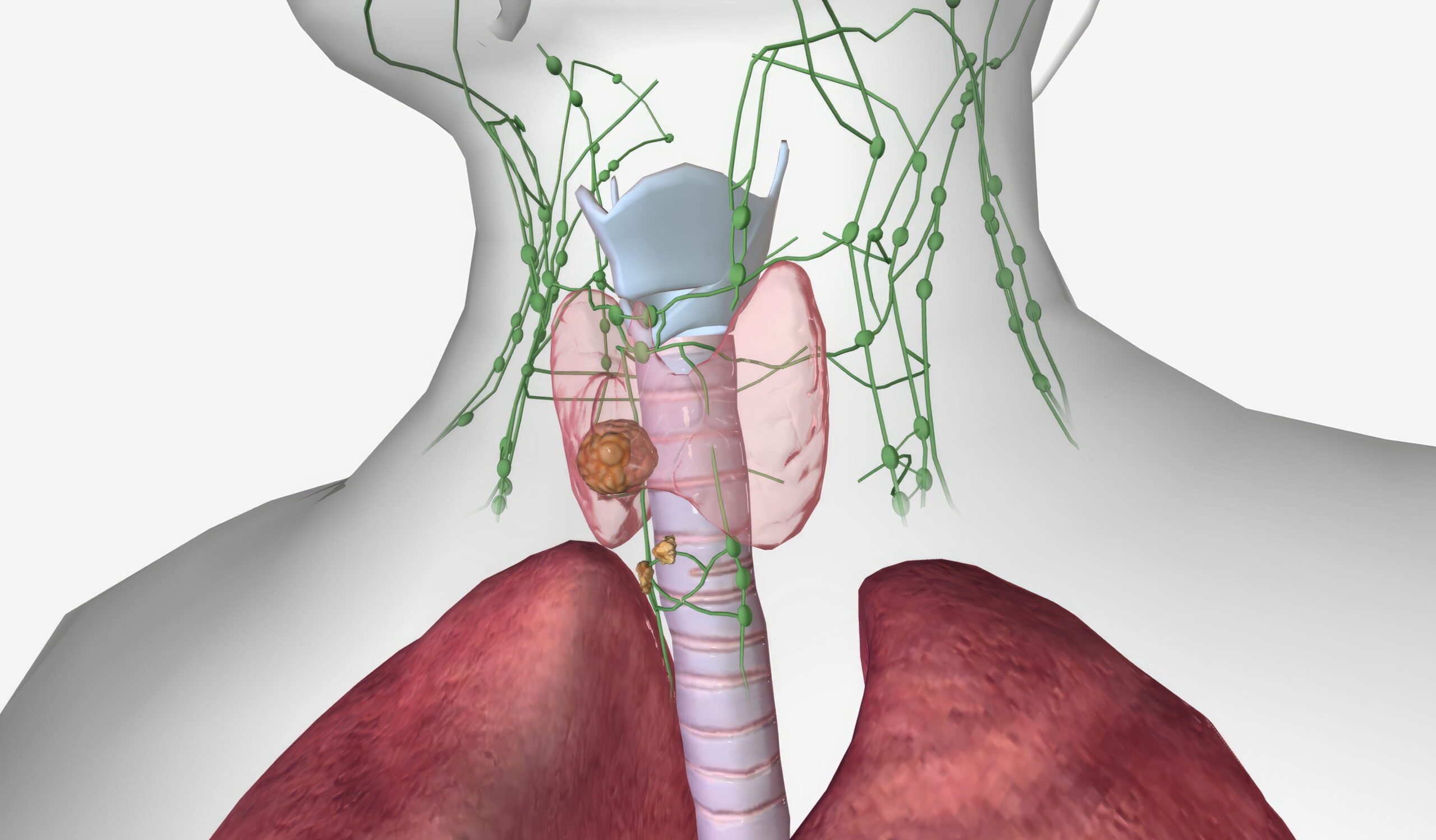
Esophageal varices are enlarged veins in the esophagus (food pipe or tube connecting the mouth to the stomach ). These veins develop when regular blood flow through the liver is obstructed by scar tissue. The damage is often the result of long-term, chronic liver damage.
Cirrhosis of the liver is the most common cause of this condition. When the liver is scarred (functional liver tissues replaced by non-functional scar tissues), the blood pressure in the portal vein rises to cause portal hypertension, which forces blood into smaller blood vessels not built for high volume. These swollen veins can leak or burst, causing life-threatening internal bleeding.
Why Do Esophageal Varices Occur?
Esophageal varices occur as a serious complication of chronic liver disease. Liver cirrhosis creates a barrier for portal blood flow. The portal venous system carries blood from the intestines to the liver. If this path is blocked, pressure in the portal system pushes blood into the veins in the esophagus.
Some people also develop gastric varices in the stomach. These are enlarged veins that form in the upper part of the stomach when portal hypertension becomes severe. As the portal venous system is connected with the stomach, in which high blood pressure can push blood into the stomach lining, creating these swollen veins.
Symptoms of Esophageal Varices
Esophageal varices are often called a silent threat because they usually cause no symptoms until they bleed internally. Most people with chronic liver disease or liver cirrhosis do not feel the enlarged veins growing inside them. However, when these veins reach a breaking point, the symptoms are sudden and severe. Esophageal varices occur silently, but a rupture is a medical emergency that requires immediate care in an advanced multispecialty setting like SRM Global Hospitals.
Signs of Active Bleeding and Rupture
If bleeding from esophageal varices begins, it is often massive and life-threatening. You must watch for these specific signs:
- Vomiting blood: This is the most direct sign of a rupture. The blood may be bright red if the bleeding is rapid. If the blood has been in the stomach for a while, it may look like dark “coffee grounds” due to stomach acid.
- Black, tarry stools: Known as melena, these stools are dark and sticky and indicate internal bleeding in the upper gastrointestinal tract.
- Dizziness and Fainting: Rapid blood loss causes a sudden drop in blood pressure and leads to lightheadedness (dizziness) or a complete loss of consciousness.
Recognising the Onset of Shock
Severe bleeding can quickly lead to hypovolemic shock, a state where the body does not have enough blood due to blood or fluid loss to keep the heart pumping. The 2025 clinical research data show that active bleeding episodes have a 20% mortality rate within the first six weeks if not managed in an emergency setting. Other symptoms of this shock include pale or cold skin, a rapid heart rate, fast breathing, and confusion.
Underlying Signs of Liver Disease
Liver specialists often suspect varices when a patient shows general signs of advanced liver disease, as portal hypertension is the invisible force driving the symptoms of these advanced-stage diseases. The signs include jaundice (yellowing of the eyes and skin) and ascites (fluid buildup in the abdomen). The 2025 clinical research suggests the 6-week mortality rate for acute bleeding in advanced liver disease is between 15% and 20%. Furthermore, patients with poor liver function face a 20% higher risk of death during a severe bleeding event.
How are Esophageal Varices Diagnosed?

Minimally Invasive Diagnosis- Endoscopy
Doctors at SRM Global Hospitals use upper endoscopy, a minimally invasive procedure on a flexible tube with a camera to find these affected veins. Regular screening via endoscopy is recommended for at-risk patients. During the exam, doctors check the veins in the oesophagus for size. Esophageal varices diagnosed this way are graded to assess the risk of bleeding. Varices larger than 5 mm or those with “red wale signs” are at the highest risk of rupture.
Red wale signs of Esophageal Varices
Red wale signs are a critical finding and the most reliable way to predict a future bleeding episode during an upper endoscopy. Research from 2025 suggests that esophageal varices with red wale signs are twice as likely to cause active bleeding compared to those without them. Doctors at SRM Global Hospitals look for these specific long, red streaks or whip-like marks on the walls of enlarged veins. These signs show the fragile veins with an immediate, high risk of bleeding. Clinical data from 2024 shows that these marks appear more frequently when portal pressure exceeds 12 mmHg.
Non-invasive Diagnosis
CT Scan
Non-invasive CT scan grading is a new 2025 method to check varices using advanced imaging and AI to view enlarged veins in the gastrointestinal tract. The scan helps to classify the size and risk of bleeding. The 2025 clinical research shows that AI-enhanced CT scans can detect high-risk esophageal varices with above 90% accuracy.
Elastography
Elastography helps doctors measure liver stiffness to predict portal pressure levels with ultrasound waves to see how much scar tissue is present in the liver, how much portal blood flow is blocked, which leads to swollen veins in the esophagus. A liver stiffness measure over 20 kPa is a strong indicator of portal hypertension.
Treatment of Esophageal Varices
Esophageal varices treatment at SRM Global Hospitals focuses on preventing bleeding and controlling active haemorrhages. As esophageal varices occur due to high pressure in the portal venous system, doctors manage the blood pressure within these blood vessels to avoid a rupture.
Preventing the First Bleed
Non-selective beta-blockers are first-line medications used to lower portal pressure and prevent variceal bleeding. The medicines narrow the arteries that supply the blood to the gastrointestinal tract to reduce portal blood flow and prevent the veins in the esophagus from bursting. Preventive treatment with these drugs is essential for anyone with enlarged veins to avoid a serious complication. The 2024 clinical data confirms that preventive treatment with beta blockers can lower the risk of a first bleeding episode up to 50%.
Emergency Bleeding Control
If active bleeding starts, the goal of treatment is to stop bleeding immediately, as it is a life-threatening situation where every minute counts.
- Endoscopic Treatment: Emergency endoscopy is preferred to stop the leak. During an upper endoscopy, a doctor uses a flexible tube to find the site of the blood loss.
- Endoscopic Banding: Also known as band ligation, this procedure uses small rubber bands to close off the bleeding veins. It is the most common way to control bleeding during an emergency.
- Sclerotherapy: In some cases, doctors inject a special solution directly into the swollen veins to make them shrink and stop the flow.
- Fluids and Transfusions: Fluids given intravenously and blood transfusions are necessary for patients with significant blood loss to maintain stable blood pressure.
- Antibiotics: These are often administered to patients with bleeding varices to prevent bacterial infections, which are common after a bleeding episode.
Advanced Medical Procedures
If severe bleeding continues despite endoscopic treatments, other steps are taken to reduce portal pressure.
- TIPS Procedure: In Transjugular Intrahepatic Portosystemic Shunt (TIPS), A specialist places a stent to reroute blood flow from the portal vein to the hepatic vein (directing to the liver). This bypass lowers the pressure in the portal venous system, which involves the stomach, intestines, spleen, and pancreas, along with the liver, almost immediately.
- Balloon Tamponade: A balloon is temporarily inflated in the esophagus to put direct pressure on the bleeding varices. It is used to buy time before more permanent medical procedures can be done.
- Liver Transplantation: Liver transplantation is the most effective way to treat the underlying chronic liver disease. It may be considered for patients with end-stage liver disease and recurrent variceal bleeding.
Managing and Preventing Liver Diseases: A Proactive Step for Esophageal Varices

Managing and preventing liver disease is a significant part of staying away from esophageal varices. Alcoholic liver disease and fatty liver disease are growing concerns in India are also called a silent epidemic. Preventing these conditions involves managing the underlying causes and keeping portal pressure low.
The Power of "Food is Medicine"
The 2025 theme for World Liver Day, “Food is Medicine,” highlights how nutrition acts as a shield for your liver from building up with non-functional scar tissue.
| Nutritional Focus | Actionable Strategy | Impact on Liver Health |
| Healthy Fats | Use olive oil or avocado oil instead of saturated fats (butter/ghee). | Protects blood vessels and reduces fat accumulation in liver cells. |
| Fiber Intake | Increase consumption of whole grains (oats, brown rice) and legumes. | Helps prevent fat buildup and maintains a healthy weight to lower portal pressure. |
| Sugar Reduction | Limit refined sugars in snacks and carbonated beverages. | Reduces the risk of fatty liver disease and metabolic insulin resistance. |
| Antioxidant Support | Incorporate turmeric, garlic, and leafy greens (spinach, fenugreek). | Activates enzymes that support liver function and reduce inflammation. |
| Oil Moderation | Reduce overall edible oil consumption by at least 10%. | Clinical data from 2025 shows that this significantly improves metabolic health in Indian adults. |
| Dietary Patterns | Follow a Mediterranean-style diet high in plant proteins. | Research from 2024 shows a 30% reduction in liver fat even without significant weight loss. |
Lifestyle Habits for a Healthy Liver
Beyond food, daily habits play a significant role in how you take care of your liver function over time.
| Lifestyle Factor | Actionable Habit | Benefit for Liver Health |
| Alcohol Consumption | Complete abstinence from alcohol. | Prevents toxins from damaging cells and stops the progress of liver cirrhosis. |
| Physical Activity | Aim for 150–300 minutes of moderate activity per week. | Improves blood flow through the portal vein and reduces stored liver fat. |
| Weight Management | Lose 7–10% of total body weight if overweight. | It can reverse early-stage fatty liver disease and improve overall liver function. |
| Toxin Awareness | Follow precise doses for drugs and pain relievers like acetaminophen. | Avoids chemical injury to reduce the risk of sudden internal bleeding. |
Life Expectancy with Esophageal Varices
Many people ask about the life expectancy for a person with esophageal varices, which largely depends on the stage of the underlying liver disease and how well the portal pressure is managed. If massive bleeding occurs frequently, the prognosis changes significantly. The 2025 clinical research shows that nearly 50% of people with liver cirrhosis have gastrointestinal varices at the time of diagnosis. Two thousand twenty-four data indicate that in advanced liver disease, the risk of new varices grows by 8-9% every year. Furthermore, bleeding varices have a 20% mortality rate for the first episode, and this risk increases significantly with end-stage liver disease. Patients who successfully control their blood pressure through medication and medical procedures can live for many years. However,
Your liver is your life!
Esophageal varices are a profound effect of chronic liver disease, which should be managed with proper care. Our liver specialists are dedicated to providing the treatment and guidance needed to extend your life with advanced liver care. Portal hypertension acts behind these enlarged veins, making early detection through endoscopy or advanced imaging tests significant.
Book your consultation at SRM Global Hospitals-trust our experts for liver care!
FAQs on Esophageal Varices
1. What causes esophageal varices to form?
Cirrhosis stands as the most common reason for these swollen veins. Thick scar tissue begins to obstruct blood flow through the liver, which raises portal vein pressure. High pressure then forces blood into smaller vessels, creating varicose veins in the food pipe.
2. Why is bleeding esophageal varices a significant risk?
Burst veins can cause life-threatening bleeding that requires urgent help. Damage happens when the link between the portal and systemic circulations is under too much strain. Doctors must reduce blood pressure in these veins to prevent future bleeding or death.
3. Can a blood clot lead to this condition?
A blood clot in the portal vein or splenic vein can block typical paths. This backup triggers high pressure even without liver scars from other liver diseases. Around 30% to 40% of people with cirrhosis will face this health issue.
4. What are gastric varices and their signs?
Swollen veins found in the stomach are called gastric varices by health experts. Vomiting blood or signs of shock show that life-threatening bleeding is happening right now. Screening stays vital for anyone with liver damage to stop such scary events early.
5. Can bleeding from varices be life-threatening?
Yes. Bleeding from varices can cause rapid blood loss, a drop in blood pressure, and lead to shock. Immediate emergence care is needed to save a life.






