Understanding Total Knee Replacement: What to Expect and Recovery Tips
Are you struggling to sit cross-legged or walk long distances due to persistent knee pain? You’re not alone. Many people across India experience knee joint issues that make daily life uncomfortable and tiring. Whether it’s pain while climbing stairs or stiffness when standing after sitting, these signs can point to more than just aging; they may hint at damaged cartilage or worn-out knee joints.
That’s where total knee replacement orthopaedic surgery becomes an option worth understanding. It’s not about shortcuts or quick fixes; it’s about reclaiming your independence, comfort, and freedom of movement. But what exactly happens during this surgery? Let’s break it down in a simple, no-jargon way.
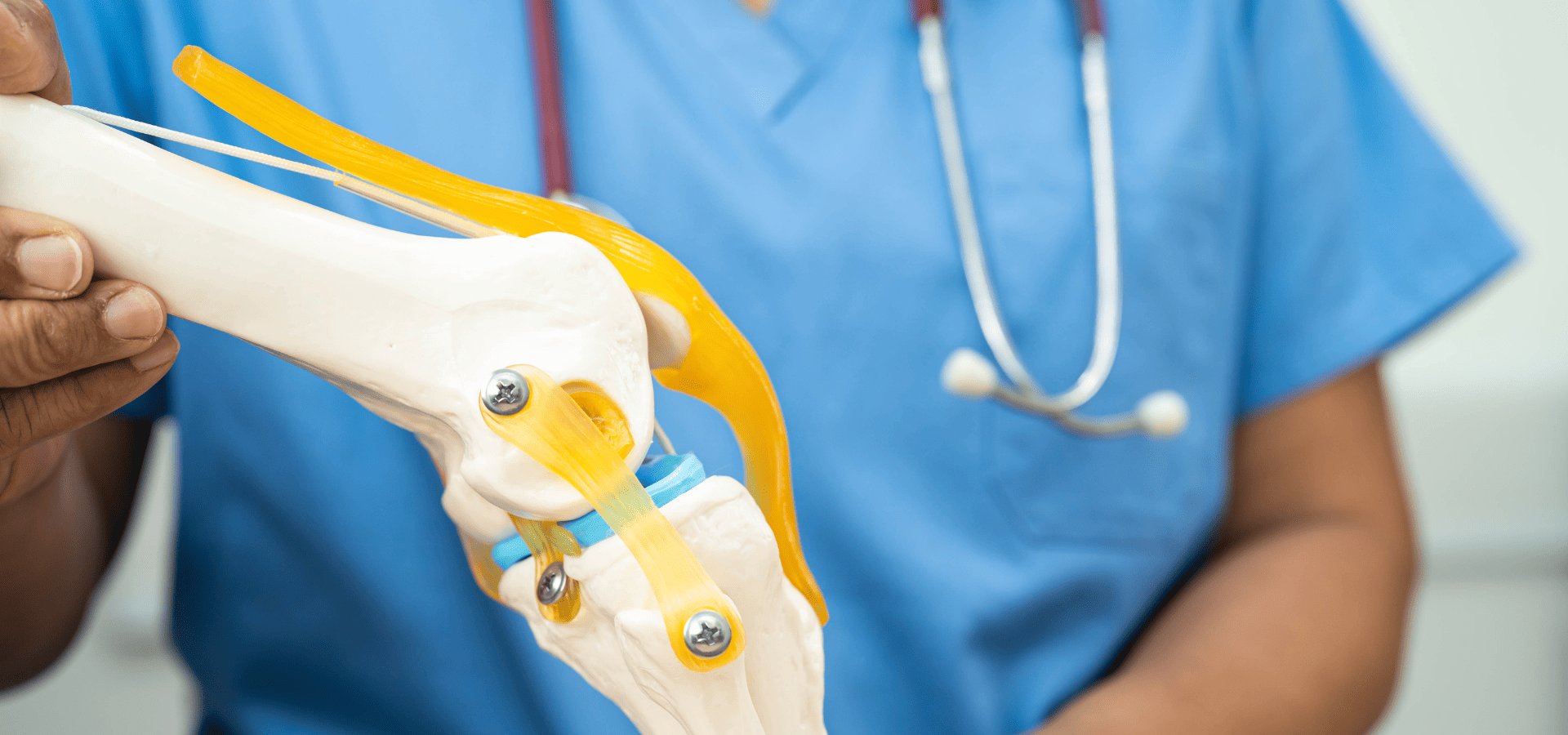
What Is Total Knee Replacement Surgery?
Total knee replacement, also called total knee arthroplasty, is a surgical procedure where the damaged parts of your knee joint are removed and replaced with metal and plastic parts. This artificial joint takes over the job of your real knee, helping you walk, climb, sit, and stand without pain.
The surgery focuses on replacing the distal femur, tibial component, and sometimes even the patella (kneecap) if it’s worn out. The goal is simple: relieve pain and restore movement.
It’s done mostly in people with knee arthritis, especially osteoarthritis, but also in those with injuries or deformities. Over time, as the joint wears out, even strong pain medications and physical therapy stop working. When that happens, total knee replacement becomes a strong solution.
Doctors use different surgical techniques, depending on your age, bone strength, and activity level. In many cases, knee replacement surgery helps improve the range of motion, ease anterior knee pain, and fix issues related to the knee’s ligaments.
What Conditions Are Treated with a Knee Replacement?
Knee replacement isn’t done for every type of knee pain. It’s mostly recommended for severe, chronic joint damage that doesn’t improve with nonsurgical treatments like medicines or injections.
Let’s explore the common conditions that lead to this decision.
1. Osteoarthritis
Osteoarthritis is the most common cause of knee replacement in India. It occurs when the articular cartilage that cushions your bones wears away due to age, injury, or obesity. With less cartilage, bones start rubbing against each other. This causes pain, swelling, and a grinding sensation when you move your leg.
Common symptoms include: Pain during activity- Stiffness in the morning, Decreased knee function, Cracking or clicking sound when walking, Unfortunately, osteoarthritis doesn’t go away. Once damaged cartilage is gone, it can’t grow back. Over time, people stop walking long distances, develop a limp, and even avoid going out. Total knee replacement helps by replacing the worn-out surface with an artificial joint, allowing smooth movement again.
2. Rheumatoid Arthritis
Unlike osteoarthritis, rheumatoid arthritis is an autoimmune condition. Your body’s immune system mistakenly attacks your joints, which can be diagnosed by orthopedic surgeons.
It often affects both knees together and causes severe inflammation. People feel pain even at rest and sometimes experience fevers or fatigue. Over time, the joint becomes deformed, and bending or straightening the knee becomes hard.
When medications like steroids and immunosuppressants stop working, surgery becomes necessary. Knee replacement in rheumatoid arthritis involves balancing soft tissue tension and using a design that can handle joint instability, like posterior stabilized implants.
3. Post-Traumatic Arthritis
This happens after a knee injury. If you’ve ever fractured your thigh bone, shin bone, or even had a patella fracture, the damage may slowly affect your knee joint.
In some cases, scar tissue forms, reducing motion. In others, the injury changes the way your bones move, causing abnormal wear. Over time, this results in arthritis.
Post-traumatic arthritis is unpredictable. It may take years to appear after a car accident, sports injury, or fall. But once pain and stiffness affect your daily life, knee replacement might be suggested.
This type of arthritis is tricky because the bones might not be aligned perfectly. Sometimes, revision surgery or minimally invasive methods are used to fix previous injuries while replacing the joint.
4. Joint Deformities and Injuries
In India, many people are born with or develop joint deformities like bowed legs or knock knees. These deformities change the way weight is distributed across the knee, wearing out one side faster than the other.
In such cases, even younger patients may feel pain, instability, and limited movement. Total or partial knee replacement can help balance the load and correct deformity.
Injuries like ligament tears (especially the posterior cruciate ligament) or untreated meniscus damage can also lead to early arthritis. Over time, pain becomes persistent, and knee replacement surgery becomes a reliable solution.
Who Should Consider Knee Replacement Surgery?
Not every person with knee pain needs knee surgery. Total knee replacement is a serious decision. Doctors check several things before suggesting it. So, how do they decide who qualifies?
Let’s break it down.
1. Pain That Doesn’t Go Away
If you feel pain even when you’re resting, sleeping, or sitting, that’s a red flag. Pain that interrupts your normal activities, even simple things like getting out of bed, using the toilet, or walking to your gate, may mean your knee joint is beyond recovery.
This pain doesn’t improve with rest, medicines, injections, or physical therapy.
2. Stiffness That Limits Movement
Do you find it hard to bend or straighten your knee fully? That’s a sign of joint damage. Severe stiffness, limited range of motion, or trouble squatting or climbing stairs means the joint is no longer functioning well.
3. Failed Non-Surgical Treatments
Doctors will first try medications, pain management, weight loss, exercises, and even joint injections. If all these fail, and you still feel pain, surgery might be the next step.
You may also be advised to use aids like braces or a firm seat cushion, or change your toilet seat riser for better comfort. But when these no longer work, replacement becomes the option.
4. X-ray or MRI Shows Severe Damage
It’s not just about pain. A physical examination is followed by imaging. If your X-ray or MRI shows damaged cartilage, bone spurs, narrowed joint space, or bone-on-bone contact, surgery is usually considered.
Doctors also evaluate alignment, the health of the knee’s ligaments, and whether you have any deformities.
5. Reduced Quality of Life
If your knee pain is stopping you from enjoying life, traveling, working, praying, attending family functions, it’s time to act. A new knee can change everything.
Most importantly, candidates should:
- Be mentally ready for surgery and recovery
- Understand risks
- Follow post-surgery guidelines
Age is not the main factor. Many patients over 70 do well. Even younger adults in their 40s or 50s may benefit if arthritis is severe.
However, people with uncontrolled diabetes, heart disease, deep vein thrombosis, or high risk factors for blood clots may not be ideal unless cleared by specialists.
If you’re unsure, consult orthopaedic surgeons who’ll evaluate if your condition calls for total knee arthroplasty or can be managed with less invasive options.
Types of Knee Replacement Procedures
Knee replacement is not one-size-fits-all. Doctors choose from several surgical options based on your knee’s condition, age, bone strength, and lifestyle. Let’s explore the different types:
1. Total vs Partial Knee Replacement
Total Knee Replacement (TKR):
In this most common type of knee arthroplasty, both sides of the knee joint (femur and tibia) are replaced with metal and plastic parts. Sometimes, the patellar resurfacing is also done. This works well for people with advanced arthritis affecting the entire knee.
- Helps in severe anterior knee pain
- Restores knee function
- Lasts 15–25 years
- High success rate in relieving pain
Partial Knee Replacement (PKR):
Here, only one side, either inner (medial) or outer (lateral), is replaced. It’s a good option if your arthritis is limited to one compartment. You retain your natural posterior cruciate ligament and more of your original bone.
Benefits:
- Smaller incision
- Faster recovery
- Less blood loss
- Preserved motion
However, it’s not suitable for those with inflammatory arthritis, knee instability, or deformities.
2. Robotic-Assisted Knee Surgery
This is modern surgery with precision. Surgeons use a robotic arm to guide them during the operation. It doesn’t perform the surgery, it assists.
Why it’s used:
- Gives real-time 3D images of the knee
- Ensures better alignment
- Reduces the risk of implant loosening
- Can reduce soft tissue damage
It’s especially helpful for younger patients, athletes, or those with unusual joint shapes. Recovery is often smoother due to better accuracy.
3. Cemented vs Uncemented Implants
Cemented Implants: Most common in India. The artificial parts are fixed using surgical bone cement. These work well for older patients or those with weaker bones.
Uncemented Implants: These have a rough surface that encourages natural bone to grow onto them. Used in younger patients with strong bone quality.
Some surgeries use hybrid techniques, where one component is cemented and the other is not.
4. Cruciate Retaining vs Posterior Stabilized
If your posterior cruciate ligament is healthy, it can be retained. This gives a more natural feel after surgery. But if it’s weak, surgeons may remove it and use a posterior stabilized implant, which has a built-in mechanism to mimic its function.
The choice depends on your joint’s stability, deformity, and the surgeon’s preference.
Benefits of Knee Replacement Surgery
If you’re wondering whether the pain, cost, and recovery of knee replacement are worth it, here’s the good news. When done at the right time and by expert orthopaedic surgeons, total knee replacement can truly change your life.
Let’s look at the key benefits during the recovery process.
1. Pain Relief
This is the #1 reason people opt for surgery. Whether it’s dull aching, sharp pain, or constant discomfort, knee pain can destroy your peace. Most people feel severe anterior knee pain while walking or even sleeping.
Knee replacement helps you:
- Relieve pain permanently
- Avoid dependence on pain medications
- Get back to daily activities pain-free
The damaged articular cartilage is removed and replaced with smooth metal and plastic parts that glide effortlessly.
2. Improved Mobility
Can’t walk to the store? Need help using the washroom? Always looking for a stable chair or safety bars?
After surgery, mobility improves within weeks:
- You can walk longer distances
- Use stairs with less support
- Move around without stiffness
- Sit and stand easily
Proper physical therapy also restores balance and gait.
3. Enhanced Quality of Life
Pain changes your personality. You avoid social functions, feel low, and slowly lose confidence.
With a new knee, life changes. You regain:
- Confidence to travel
- Ability to work and support your family
- Better sleep and energy levels
- More independence
You no longer worry about falling, struggling with chairs, or avoiding outings.
4. Long-Term Success Rates
Modern total knee arthroplasty has high success. In fact, 90–95% of implants last 15–20 years. Some even last longer with good care.
Younger patients may need a revision surgery later, but for most, the benefits last a long time.
Also:
- Better designs are available now (like posterior stabilized and cruciate retaining)
- New surgical techniques reduce errors and speed up healing
- Robotic-assisted surgeries improve alignment and balance
Risks and Complications of Knee Replacement
Like all major surgeries, knee replacement has some risks. But don’t panic, most problems are preventable when surgery is done in expert hands and proper care is taken before and after.
Let’s discuss the main complications you should know, especially after the recovery room.
1. Infection
Even with best practices, infections can occur, either at the incision site or deep around the artificial joint.
Signs include:
- Fever
- Redness and swelling
- Drainage from the wound
- Pain that worsens suddenly
To reduce risk:
- Follow post-op hygiene instructions
- Avoid touching the wound
- Complete your antibiotic course
- Report any fever immediately
In rare cases, deep infections may need additional surgery.
2. Blood Clots
After surgery, blood clots can form in the legs (known as deep vein thrombosis). If these travel to the lungs, they can cause serious issues.
To prevent clots:
- Wear support stockings
- Start walking early
- Do leg exercises
- Take blood thinners if prescribed
Let your doctor know if you feel swelling, warmth, or pain in your calf.
3. Implant Loosening or Failure
With time, the femoral component or tibial component of your implant may loosen. This can happen due to poor alignment, infections, or wear and tear.
Loosening causes pain, reduced function, and instability. If severe, a second surgery may be needed. This is called revision surgery.
To reduce risks:
- Keep weight in control
- Avoid high-impact sports
- Attend regular check-ups
- Report any new knee pain
4. Stiffness and Limited Motion
Sometimes, scar tissue forms around the joint and limits bending or straightening. This is more common if you delay rehab.
Stiffness can be managed with:
- Aggressive physical therapy
- Continuous motion exercises
- In rare cases, another surgery to break scar bands
Early movement is key. Use aids like walkers or toilet risers, but don’t avoid motion.
Other Risks
- Patella fracture during surgery
- Anterior femoral notching can weaken the bone
- Soft tissue imbalance may cause instability
- In rare cases, an allergic reaction to the implant material
However, these are uncommon if you choose skilled orthopaedic surgeons and follow instructions during recovery.
How Long Does It Take to Recover from Knee Replacement?
Recovery isn’t instant. It takes time, effort, and patience. But if you follow the plan, you’ll feel stronger and more mobile with each passing week.
Let’s look at the timeline in phases.
Week 1: Immediate Post-Surgery
- You’ll be in the recovery room for a few hours after surgery.
- Pain is managed with medications and ice packs.
- Physical therapy starts the same day or the next morning.
- You’ll begin walking with a walker and doing light movements.
Important: Avoid falls. Use a stable chair, firm seat cushion, and always sit with knees straight.
Weeks 2–4: Early Recovery
- You’ll be discharged from the hospital (usually after 3–5 days).
- Staples or stitches will be removed.
- Walking gets easier, though you’ll still use crutches or a walker.
- A physical therapist will visit or guide you with in-home exercises.
Continue:
- Leg raises
- Heel slides
- Knee bends
- Ankle pumps
Weeks 4–8: Regaining Strength
- Walking without support may start
- Climbing stairs with help
- Focus on regaining range of motion and soft tissue healing
- You may resume light chores
Still avoid:
- Sitting on low sofas
- Cross-legged positions
- Wet bathroom floors
Use safety bars and support stockings to reduce swelling and prevent blood clots.
2–3 Months: More Activity
- You can walk independently
- Drive if the knee bends well and pain is under control
- Return to light work (especially desk jobs)
- Swelling has reduced a lot by now
Continue physical therapy and stay active without overdoing it.
3–6 Months: Normal Life Returns
- Travel, attend functions, visit relatives
- Full knee bending and strength possible
- Swelling almost gone
- Resume most daily routines
By now, your new knee feels part of you.
After 6 Months: Long-Term Recovery
- Sports like walking, swimming, and cycling are okay
- Avoid jumping, running, or twisting moves
- Total knee settles and continues to improve
Most people feel like themselves again by 9–12 months. But full healing and knee function may take a year.
Preparing Yourself for Surgery: What to Do Before the Operation
The better you prepare, the smoother your surgery and recovery. Start planning 3–4 weeks before surgery.
1. Medical Evaluation and Imaging
Your doctor will:
- Take a detailed medical history
- Do a physical examination of your knee
- Order blood tests, ECG, chest X-ray
- Take X-rays or MRI of your knee
Why? To confirm if you need total knee replacement or partial knee replacement, and to rule out risks like heart disease or blood clots.
Also inform them if you take:
- Blood thinners
- Diabetes medications
- Herbal supplements
You may need to stop some medicines before surgery.
2. Prehab: Strengthening and Stretching
Start light exercises 2–3 weeks before surgery:
- Straight leg raises
- Quad sets
- Ankle pumps
- Hamstring stretches
This helps strengthen your thigh and calf muscles. Stronger muscles mean faster recovery.
Also, learn how to:
- Use a walker
- Get out of bed safely
- Climb stairs with support
A physical therapist can train you.
3. Home Setup and Caregiver Support
Your home needs to be surgery-ready.
Do this before your surgery:
- Remove loose carpets and clutter
- Install safety bars in the bathroom
- Use a toilet seat riser
- Arrange a stable chair with arms and a cushion
- Set up your bedroom on the ground floor
Also, stock up:
- Dry fruits, fruits, and home-cooked meals
- Clean towels and soft clothes
- Medications and wound care items
Arrange someone to:
- Stay with you during your hospital stay
- Help with cooking and bathing
- Drive you to therapy or hospital visits
Good planning saves stress later.
What to Expect During Your Hospital Stay
Your hospital stay is short, usually 3 to 5 days. But these first few days are critical.
1. Monitoring and Pain Control
- Nurses monitor your vitals every few hours.
- Pain is managed with IV medicines, oral tablets, or injections.
- Cold packs help with swelling.
- The incision site is checked for bleeding, infection, or signs of deep infection.
2. Early Movement and Walking
You’ll be encouraged to:
- Sit on the bed edge the same day
- Stand with support by Day 1
- Start walking short distances with a walker by Day 2
This helps:
- Prevent blood clots
- Improve circulation
- Avoid stiffness and scar tissue
You’ll be trained on:
- Getting in/out of bed safely
- Using a walker or crutches
- Basic physical therapy exercises
3. Preventing Complications
To reduce the risk of problems:
- You’ll wear support stockings to prevent swelling
- Leg pumps or foot movements help blood flow
- Antibiotics prevent infections
- Blood thinners prevent clots
Doctors also guide you about your diet, light, nutritious, and low in salt or sugar.
Before discharge, you’ll get:
- Instructions for wound care
- Medications list
- Physiotherapy schedule
- Follow-up appointment
Your caregivers are also briefed on:
- Using a toilet seat riser
- Elevating legs
- Safe ways to help without hurting themselves
Physical Therapy and Rehabilitation
If you want the best result from your total knee replacement, there’s one thing you can’t ignore: physical therapy. It’s not optional. It’s essential. Rehab is what brings your joint back to life.
Physical therapy begins just hours after surgery and continues for months. In the early days, your therapist will guide you through simple exercises. These include ankle pumps, leg lifts, heel slides, and bending the knee slowly. These may look small, but they’re powerful. They prevent scar tissue, improve range of motion, and build strength.
The first goal is to bend the knee to at least 90 degrees and straighten it fully. You’ll start with short walks, first with a walker, then with a cane, and finally without support. Your therapist will also help you learn how to climb stairs safely and sit in a chair without stressing your joints.
As you heal, therapy progresses. You’ll add resistance bands, step-ups, and even mild cycling. These improve muscle control, balance, and joint endurance. Focus will shift from just movement to confident movement. If you’re someone who used to limp or drag your leg before surgery, your walking pattern will now be corrected.
Therapy can be done in two ways, in-clinic or home-based. Home therapy works well for the first few weeks. But visiting a rehab center or clinic offers better tools,expert supervision, and peer motivation. If possible, try both.
There will be days when you won’t want to do your exercises. Days when pain holds you back. But skipping therapy is like skipping healing. Think of your physical therapist as your coach. Trust the process, follow the plan, and your knee function will improve more than you thought possible.
By the end of three months, your strength, flexibility, and confidence will be miles ahead. You’ll walk into a room, not limp into it. And that is the true win of knee arthroplasty.
Tips for a Smooth Recovery at Home
Coming home after knee replacement surgery is both exciting and stressful. You’re finally out of the hospital, but now the responsibility of healing is in your hands. Small, everyday decisions will either help or hurt your recovery. Let’s focus on getting it right.
First, create a safe and simple home layout. Clear pathways and remove loose carpets or any clutter that could make you trip. Use a stable chair with a high seat and armrests to sit down and get up without stress. A toilet seat riser in the bathroom and safety bars near the shower can help more than you think. These minor changes reduce fall risk and make movement safer.
Pain and swelling are your body’s natural reaction to surgery. But they can slow you down. You need to stay ahead of the discomfort. Follow this daily plan:
- Apply ice packs for 15–20 minutes every few hours
- Take pain medications on time, not after the pain starts
- Elevate your leg using pillows under your calf (not knee) to reduce swelling
- Wear support stockings if advised to prevent blood clots
- Keep the incision clean and dry; don’t apply creams or powders unless told
Use your walker or cane properly. Don’t rush to walk without support. Keep the device close to your body and take small steps. Avoid climbing stairs unless guided by a therapist. If stairs are unavoidable, always use a railing and go slowly.
Ease back into your routine slowly. Start by:
- Brushing, bathing, and dressing on your own
- Moving from bed to chair without help
- Sitting for meals with family
- Taking a few steps every hour to avoid stiffness
Also, don’t ignore your emotional well-being. Healing can be frustrating. You may feel weak or tired. But remember, each day, your body is doing hard work inside. Be patient with yourself.
Ask a family member to assist you for at least the first 2–3 weeks. Whether it’s helping with meals, laundry, or getting medicines, a helping hand makes healing smoother. Make sure you have your doctor’s phone number handy for emergencies or unusual symptoms.
Consistency is your best friend during recovery. Do your exercises. Take your meds. Rest without oversleeping. Walk without overdoing. These small habits bring big results.
Diet and Nutrition for Faster Healing
What you eat after total knee replacement surgery can speed up healing, reduce swelling, and even prevent infections. Your body is like a construction site after surgery, and it needs strong materials to rebuild tissue, bones, and energy.
Start with protein-rich foods. Protein repairs tissues and builds muscles, which are crucial for getting back strength around your new knee.
Best protein options to help replace damaged cartilage :
- Dals and legumes
- Paneer, curd, and milk
- Eggs (boiled or poached)
- Chicken or fish (lightly cooked)
- Soya, tofu, and sprouts
Next, focus on anti-inflammatory foods. These help reduce pain and internal swelling.
Add these to your plate:
- Turmeric (haldi) in warm milk or food
- Ginger (adrak) in tea or sabzi
- Garlic, which boosts immunity
- Fresh fruits like papaya, pineapple, and oranges
- Green leafy vegetables like spinach and methi
Avoid junk food, processed snacks, and too much salt. They slow healing and increase water retention, making your leg feel heavy.
Hydration matters. Drink 8–10 glasses of water daily. Add coconut water, buttermilk, and fresh juices for variety. Avoid fizzy drinks or packed juices.
To help bone strength, get enough calcium and Vitamin D:
- Milk, curd, and cheese
- Ragi, sesame seeds, and almonds
- Sunlight for 15 minutes every morning
- Doctor-prescribed supplements, if needed
Energy is another piece of the puzzle. After surgery, many feel tired even after light activity. That’s normal. But skipping meals or eating late won’t help.
Maintain a balanced meal plan:
- Small, frequent meals
- Include rice, rotis, fruits, and vegetables
- Avoid spicy, oily, or heavy foods
Here’s a sample post-op meal idea:
Breakfast: Moong dal chilla + curd + banana
Lunch: Rice + dal + spinach sabzi + salad
Evening: Coconut water + roasted chana
Dinner: Vegetable khichdi + soup
A good diet won’t replace therapy or medicines. But it will give your body the energy and materials it needs to heal properly.
When Can You Get Back to Normal Life?
Everyone wants to know: “When will I feel normal again?” The answer is – slowly, but surely. Life after total knee replacement gets better with time. But don’t rush. Healing is personal. Your age, health, commitment to rehab, and even mindset matter.
The first few weeks after surgery are for rest and routine. After that, recovery becomes about action. Let’s look at common milestones.
1. Walking
Most patients start walking with a walker within 1–2 days post-surgery. By 3–4 weeks, many shift to a stick. You’ll walk independently by 6–8 weeks if recovery goes well.
Tip: Walk often, not fast. Short walks several times a day help more than long walks once a day.
2. Climbing Stairs
By 3–4 weeks, you’ll begin gentle stair practice. Always use the railing. Go slow. Don’t skip steps. One foot at a time.
Rule: “Up with the good, down with the bad.” Use your stronger leg first when going up. Use the operated leg first when going down.
3. Driving
You can usually drive by 6–8 weeks, but only if:
- Pain is under control
- You can bend your knee comfortably
- You can press the brake and clutch safely
- You’re off painkillers that cause drowsiness
Check with your doctor before starting.
4. Work
Desk jobs may resume in 6–8 weeks. Field jobs or standing work may take 3 months. Jobs involving heavy lifting or long travel may need more time or adjustments.
Tip: Use a firm seat cushion and take standing breaks every 30 minutes.
5. Travel
Short car rides can begin by 4–6 weeks. Long journeys, especially flights, may require support stockings and frequent leg movements to avoid blood clots. Carry your medications and sit in a comfortable position.
Avoid travel in early monsoons or flu season to lower infection risks.
6. Exercise and Sports
You can:
- Walk
- Cycle on a stationary bike
- Swim (after the wound heals)
- Do light yoga and stretching
Avoid:
- Jumping
- Running
- Contact sports
- Cross-legged sitting or squatting on the floor
These put extra strain on your artificial joint and reduce its lifespan.
Your new knee will support most daily activities. Just give it time, and treat it with care.
Long-Term Care for Your New Knee
The surgery is just one part of your journey. Long-term success depends on how you treat your knee after the hospital and rehab are done. Here’s how to protect your implant and stay pain-free for years.
1. Maintain a Healthy Weight
Extra body weight puts pressure on your tibial component, wears out the plastic spacer faster, and increases the risk of aseptic loosening.
Solution:
- Eat light, clean meals
- Walk daily
- Avoid sugary snacks and soft drinks
2. Keep Moving
Movement prevents stiffness and keeps muscles strong.
Make a habit of:
- Walking 20–30 minutes daily
- Light stretching every morning
- Doing some rehab exercises weekly
This keeps your knee function smooth and stable.
3. Watch for Signs of Trouble
You should contact your doctor if you notice:
- New swelling
- Pain that returns suddenly
- Clicking or popping sounds
- Redness or warmth around the knee
- Difficulty bending or straightening
These may signal implant loosening, infection, or soft tissue issues.
4. Attend Regular Follow-ups
Your orthopedic team will track your knee’s progress with X-rays and checks. Usually:
- 6 weeks after surgery
- 3 months
- 6 months
- Once a year after that
This helps catch any small issue before it becomes a big problem.
5. Protect Against Falls
Falls are the enemy of a new knee.
Stay safe by:
- Wearing non-slip footwear
- Keeping your house clutter-free
- Avoiding wet floors
- Using support bars where needed
Also, avoid sitting on very low surfaces, which stresses the knee when getting up.
6. Implant Lifespan
Most modern implants last 15–25 years. You can extend this by:
- Avoiding jerky movements
- Keeping your bones strong with calcium and Vitamin D
- Staying active without overstraining
A revision surgery may be needed later in life. But with good care, many patients never require it.
SRM Global Hospitals – Your Partner in Safe and Successful Knee Replacement
Choosing where you get your knee replacement surgery is just as important as deciding to have the procedure in the first place. You need more than just a hospital; you need a care partner. That’s where SRM Global Hospitals comes in.
At SRM Global Hospitals, we bring together top orthopaedic surgeons, advanced surgical technology, and a deeply personalised patient care system. Whether you’re dealing with rheumatoid arthritis, osteoarthritis, or complex post-traumatic joint issues, our expert team has the experience to handle every case with precision and compassion.
Why Patients Trust SRM Global Hospitals for Knee Surgery:
- Experienced Specialists: Our orthopedic team has decades of hands-on experience in total knee arthroplasty, partial knee replacement, and revision surgeries.
- Advanced Techniques: We offer modern surgical options, including robotic-assisted knee replacement, minimally invasive procedures, and the use of cemented or uncemented implants based on individual patient needs.
- Infection Control & Safety Protocols: We follow strict guidelines to reduce the risk of deep infections, blood clots, and post-surgical complications.
- Personalised Rehab Plans: Our physical therapists create tailored recovery programs to restore range of motion, knee function, and improve patient outcomes quickly and safely.
- Holistic Support: From your first consultation to your last follow-up, you’ll be supported by a team that truly cares, whether it’s for pain control, emotional support, or caregiver education.
You deserve care that’s reliable, transparent, and rooted in proven results. At SRM, your comfort, safety, and confidence are always our first priority.
Book Your Appointment Today
Don’t let knee pain control your life. If you’re tired of temporary fixes and want a lasting solution, it’s time to talk to our specialists. Let’s help you move freely again, with less pain, better balance, and full confidence in every step.
Call us now to schedule a consultation with our senior orthopaedic surgeons
Visit the nearest SRM Global Hospital
Or book online through our official website – it only takes a minute
Your journey toward a pain-free life starts here, with people who truly understand what it takes.
FAQs
1: How long does a total knee replacement last?
A well-done surgery with good care usually lasts 15–25 years. Many patients never need a second surgery, especially if they follow rehab and avoid high-impact activities.
2: Can both knees be replaced at once?
Yes, if you’re healthy and fit, both knees can be replaced in one sitting. However, the doctor may suggest one knee at a time based on your risk factors.
3: Will I be able to sit cross-legged or squat after surgery?
No. Sitting cross-legged or squatting puts strain on the artificial joint. These positions should be avoided to protect your implant and ensure long-term success.
4: Is knee replacement very painful?
Mild pain is normal after surgery, but it’s well-managed with medications and therapy. Most patients say the recovery pain is far better than the arthritis pain they lived with.
5: What is the best age for knee replacement?
There is no fixed age. If your knee pain affects daily life and all nonsurgical treatments fail, you could be a good candidate, even in your 40s or 80s.






